Nutrition and Brain Function
Boosting Our Knowledge of Brain Food
|
|
Aging. While everybody’s doing it at the same time, some people are more successful at forestalling its effects on cognition, or mental agility, than others. Cognitive function is measured by the level at which the brain is able to manage and use available information for activities of daily life.
“Loss of cognitive ability robs quality of life and independence,” says ARS-funded physician Irwin H. Rosenberg, who heads the Nutrition and Neurocognition Laboratory at the Jean Mayer USDA Human Nutrition Research Center on Aging (HNRCA) at Tufts University in Boston, Massachusetts. “As the world population grows and the number of senior citizens increases, dementia is becoming a big problem.”
Dementia is the progressive decline in cognitive function—such as memory, attention, language, and problem solving—due to a diseased or damaged brain rather than to normal aging.
“The fact that many individuals maintain their full mental faculties into old age suggests that cognitive decline is not a necessary feature of normal aging,” says Rosenberg. “But aging may affect the brain’s need for nutrients that are involved in normal brain metabolism, such as synthesis of neurotransmitters and maintenance of brain-cell signaling, connectivity, and repair capacity.” Adjusting dietary intake of certain nutrients could eventually prove to be key to forestalling cognitive decline.
At some point, there will be more people in the United States older than age 65 than there are children, according to estimates. Researchers at HNRCA have been conducting intervention trials, population studies, and laboratory tests to learn how a variety of nutrients and biochemicals affect cognitive decline for this growing demographic group.
Homocysteine: A Suspect Biomolecule
Several HNRCA researchers are looking into whether elevated blood levels of the amino acid homocysteine are involved in cognitive decline—and if so, how.
Homocysteine is a byproduct of the body’s metabolism of methionine, an essential amino acid. Unlike other amino acids, homocysteine is not used by the body to build protein. Instead, it can be converted back to methionine or to cysteine, another amino acid, through a reaction with certain B vitamins. In individuals with deficiencies in those particular B vitamins, homocysteine may accumulate in the blood. This buildup is suspected to irritate blood vessel linings and encourage the development of atherosclerosis, or “hardening of the arteries.”
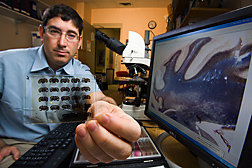
At HNRCA, neurobiologist Aron Troen has been studying laboratory mice to understand how nutrition might affect age-related cognitive decline in humans. “We are looking at the impact of nutrition on brain blood vessels, chemistry, and other pathways,” he says. One of his recent studies suggests that all cases of high homocysteine may not have the same effects on the body’s organs.
Troen fed young mice genetically predisposed to atherosclerosis one of four diets with differing B-vitamin and methionine contents for 8 weeks. Troen then conducted psychomotor, spatial, memory, and learning tests with the mice. He found that low B-vitamin intake was associated with memory and learning dysfunction, whereas excess methionine intake was associated with accelerated blood vessel disease.
“This suggests that different nutritional impairments leading to high homocysteine levels may also lead to different end-organ dysfunctions,” says Troen. “The diets that led to cognitive deficits were different from those that led to further vascular disease.”